The Age 18 June 2019
Victoria is on the verge of allowing terminally ill people to lawfully end their lives.
The historic law, which was passed in November 2017 after a state parliamentary inquiry into end-of-life choices, and a ministerial advisory panel on voluntary assisted dying, comes into effect on Wednesday, June 19.
While Victoria is not the first jurisdiction in the world to offer some form of assisted death, the bill – which contains 68 safeguards – has been described as the most conservative of its kind.
So how will it work?
Who can use the laws?
Voluntary assisted dying will be available only to Victorians who are over the age of 18. The patient must be capable of making sound decisions, give informed consent and communicate their decision.
They must be diagnosed with an incurable disease or a condition that causes intolerable, unrelieved suffering, and must be expected to live for fewer than six months – or no more than 12 months, for those with a neurodegenerative diagnosis.
They must have lived in Victoria for at least one year before making a first request for voluntary assisted dying, and be an Australian citizen or permanent resident.
The person choosing to end their life must be the one to make the decision to access the laws and it cannot be made by anyone else on their behalf.
Having dementia is not a sufficient reason for a person to access voluntary assisted dying (the same as disability or mental illness).
A person diagnosed with dementia, however, may be eligible if they meet all of the criteria, including having decision-making ability throughout the entire process.
What are the steps to using the laws?
A terminally ill patient must make three, clear requests.
Firstly, they must make a verbal request about voluntary assisted dying to their doctor (generally, their GP). This conversation must be initiated by the patient and no one else. The doctor cannot raise the issue of assisted dying with a patient. Doctors who suggest the assisted dying scheme to patients face a professional misconduct investigation.
This doctor is called a”co-ordinating doctor” and it is their job to assess the patient to determine their eligibility for the scheme in the first instance.
Once they’ve been assessed, a patient must then make a second request to a different doctor, in the form of a written declaration, signed in the presence of two witnesses and their co-ordinating doctor.
The second doctor, generally a specialist in the person’s illness, called a “consulting medical practitioner,” will then conduct another assessment of the patient to confirm their eligibility.
Once this is complete, the patient must make a third and final verbal request to the co-ordinating doctor. This must be at least nine days after the first request (unless death is likely to occur before).
The co-ordinating doctor will then conduct a final review to certify the request and assessment process.
They will then apply for a voluntary assisted dying permit, either for self-administration or practitioner administration, depending on the patient’s circumstances.
The application is handed to the Victorian Department of Health and Human Services, which reviews and approves all requests for voluntary assisted dying.
The law outlines a period of 10 days between the first request to a doctor and being given the means to end life. This means that the first person to take their own lives legally in Victoria could do so on June 29.
At any stage of the process, a person who has requested access to assisted dying may change their mind and decide not to proceed.
How would the lethal drug be administered?
A small team of pharmacists at The Alfred hospital will have sole responsibility for preparing and supplying all the required drugs for the lethal substance.
The drugs needed to make the lethal dose are already legal in Australia; there will be no need to import the banned euthanasia drug pentobarbital.
Authorities made the decision to have a single point of access for the euthanasia drug rather than having it dispensed from multiple pharmacies to ensure that patients are provided with consistent information, and that unused medications are returned and destroyed.
The pharmacists will travel around the state to dispense the medication to patients. The lethal substance will be handed to patients in a locked box.
Most people will drink the dose – a liquid of about 100 millilitres (just over a third of a cup) – in their own homes at a time of their choosing.
Those ending their lives will also be given medication to relax and reduce any chance of regurgitation before they take the lethal substance, which will cause unconsciousness within minutes and a peaceful, pain-free death soon after.
Under certain circumstances, those physically incapable of swallowing will be allowed to take the substance as a lethal intravenous drip set up by a doctor.
Nobody else, including the pharmacist delivering the lethal substance, is permitted to administer the drugs.
If someone breaches the self-administration permit, they face potential life imprisonment. Anyone who induces a person to request assisted dying faces up to five years jail.
The patient must appoint a person who will return any unused medication to The Alfred if they die before taking the lethal substance, or decide not to take it.
A pharmacist can also retrieve the the unused medication and take it back to The Alfred. Unused lethal medication must be returned within 15 days of death.
What should we call it?
Language around the issue has long been a battlefield.
In framing the Victorian bill, serious consideration was given before the words “voluntary assisted dying” were chosen.
The Ministerial Advisory Panel on Voluntary Assisted Dying found there was a “significant social stigma” attached to the term “suicide'” and for this reason, determined that “assisted suicide” was not an appropriate term.
While, technically, a terminally ill person who takes a lethal drug has still died by suicide, the distinction is important, say supporters of the law, because the word carries enormous emotional weight.
Suicide, they argue, connotes a violent death, usually carried out by someone suffering from depression or a mental illness that might feasibly have been treated.
By contrast, “voluntary assisted dying” is about a decision made by a terminally ill person in full command of their mental faculties. It’s about someone who is already dying choosing to end their suffering, supporters say.
The advisory panel also ruled out “dying with dignity” on the basis that it implied only those who opted for assisted dying were taking a dignified path.
Many opponents of the Victorian bill still use the phrase “assisted suicide”, including the Catholic Church and the Australian Medical Association, which calls it “physician-assisted suicide”. (The Victorian chapter of the AMA, however, calls it “physician-assisted dying”.)
Euthanasia is a broad umbrella term for a range of different practices for ending a person’s life, some of which Victoria’s legislation doesn’t allow for.
At The Age we use the term euthanasia to refer to the issue, while we use the term assisted dying in relation to the laws.
The term euthanasia comes from the Greek word euthanatos, which can be translated as “easy death” and is defined as the painless killing of a patient suffering from an incurable and painful disease.
It is important to note, however, the word euthanasia is not written anywhere in the state’s legislation.
What checks and balances would be in place?
A Voluntary Assisted Dying Review Board has been established to review each assessment that has been approved.
The board is chaired by a retired judge of the Supreme and County courts, Betty King, and has 12 other members ranging from palliative care specialists to neurologists, oncologists, pharmacists and doctors.
The board’s role is not to grant or refuse applications for voluntary assisted dying. Its purpose is to review each case retrospectively to ensure that laws haven’t been breached.
Doctors breaking the law would be likely to be quickly exposed as every assessment for euthanasia, positive or negative, will be reviewed by the board.
The board can refer breaches to the police, coroner or the Australian Health Practitioner Regulation Agency.
The patient’s terminal illness will be listed as their underlying condition but the voluntary assisted dying act will be recorded as the cause of death on their death certificate and in the register.
Can doctors object to helping someone end their life?
Any health practitioner can “conscientiously object” to participating in any part of the euthanasia process. But they would not be allowed to impede someone’s access to the regime.
The Victorian Department of Health has established a training body capable of preparing medical specialists wanting to assist voluntary dying. All doctors who want to be part of the scheme must undertake this training.
To date, about 100 doctors including GPs, cancer specialists and palliative care clinicians have undertaken mandatory, specialist training ahead of the laws being enacted.
About a third of those doctors are from regional Victoria.
How many people are expected to apply for assisted dying?
It has been estimated that about 150 Victorians could make use of euthanasia laws each year but the state government predicts the number could be as low as 12 in the first year – experience in other places where euthanasia is legalised shows that the initial take-up can be slow.
In the US state of Oregon in 1998, after a Death with Dignity Act first came into force, 24 terminally ill people took the option to end their lives. Since then, the number has risen steadily, peaking at 218 deaths in 2015.
The Northern Territory parliament passed the Rights of the Terminally Ill Act, to allow assisted dying, in 1995 but it was overturned in 1997. Under the short-lived legislation, four people, including two terminally ill patients from NSW and South Australia, ended their lives.
Queensland and Western Australia are now considering enacting voluntary assisted dying legislation.
https://www.theage.com.au/national/victoria/how-victoria-s-assisted-dying-laws-work-20190523-p51qeb.html
 Keep up with family issues in NZ.
Keep up with family issues in NZ.
Receive our weekly emails direct to your Inbox.
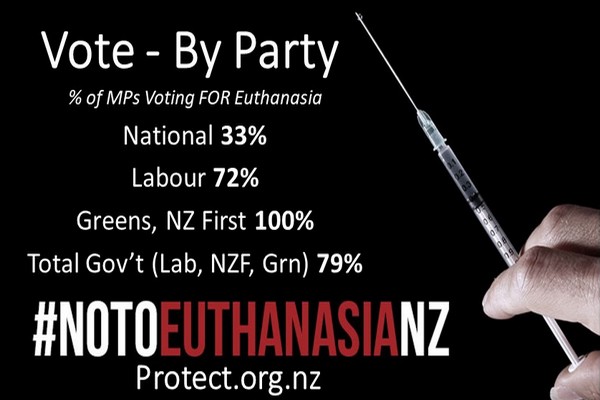
 National
National![]() NO
NO Labour
Labour![]() NO!
NO! NZ First
NZ First YES (All MPs!)
YES (All MPs!)