The Maxim Institute’s Research Manager, Maryanne Spurdle, joins Simon to discuss her latest research – Interrogating Choice: Euthanasia and the illusion of autonomy. Simon and Maryanne discuss how the underfunding of palliative care is removing genuine choices from individuals at the end of life. They also talk about the increased push by the likes of the Ministry of Health and others to remove doctors, nurses, and hospices’ conscience rights – that is, force people to participate in something they do not want too.
To read Maryanne’s paper: https://www.maxim.org.nz/article/interrogating-choice-euthanasia-and-the-illusion-of-autonomy/
TRANSCRIPT:
Simon: Hi everyone. Great to have you back here on The Family Matters podcast. As I always say, we are going all around the world, but we’re back in New Zealand this week. I’m very pleased to bring back on to the podcast Marian Spurtle, she’s now the research manager at the Maxim Institute has been part of the research team, but now we are managing it Maryanne.
So congratulations on that.
Maryanne: Oh, thank you. Good to be with you.
Simon: Well, good to have you back. Last time we were talking education this time we are, we’re still speaking in a space beginning with e but a heavier topic particularly around euthanasia, but broader than that conscience rights autonomy freedom, palliative care and so on.
But the reason is because you’ve just released a discussion paper called Interrogating Choice Euthanasia. And the illusion of autonomy hence bringing you on the show. So give us a quick introduction for those who, well, first and foremost, they should go onto the Maxim website and read it. It’s only 23 pages.
And can I say easy to read but give viewers a bit of a sense of what this paper’s about.
Maryanne: Yep. Well, as we’re all aware now, euthanasia is legal. It has been frigid over three years, and the Ministry of Health, one of the requirements of the law is that after it was in effect for three years, they had to do a survey of how it was going and publish a report.
So that came out last November, and it was interesting reading. If you take it at face value, it’s saying the legislation is working fine. We just have a few little glitches to work out. But when you look into the problems with how it’s being well, I mean the, there are problems with. The fact that there’s now a legal way to kill people, that immediately brings up challenges, but the actual way it’s being implemented doesn’t match the way it is on paper.
So on paper there’s a review committee that checks things after they’ve happened and make sure that yep, ev everything is aligning with the legislation. Before the review even came out, two of the former reviewers publicly expressed concerns. So I’ll go into a little bit of that. That’s in the paper.
So it’s not even lining up with the legislation. And now we’ve got the Ministry of Health Review. It’s suggesting some changes, some of which are to close gaps but most of which are to expand access, make access easier for people who want to and the trouble is that’s an intention with safety.
As soon as you make something. Easier to access, you make it less safe when it’s something that, that has risks like coercion. So my paper is looking at first of all, what in the legislation is problematic because it’s called End of Life Choice Act. How good is the choice it offers? And then given the ministry’s view of how it’s been implemented and what, what should change?
Does that actually assist choice or does it limit choices for people de despite what it says in you know, face value, the word is choice, but is it,
Simon: which, you know, spoiler alert from my side what they’re suggesting, and I think what you will not think, I know what your papers said is actually going to limit.
Choice. In fact, one thing that struck me amongst many you discussed well, one of the recommendations or suggestions put to the ministry and the review was to have this cooling off period to give people a little bit more time to ponder the early termination of their life. And the ministry ultimately said, no.
We understand it will make things safer but it won’t facilitate access. This equity of access just kept coming on through. So in many ways that they’re happy to. Reduce that choice decrease safety, just to make this more, I think you used the word somewhere in the port to normalize euthanasia, and that struck me as something in their review.
Maryanne they very much want to normalize.
Maryanne: That’s their words as well, not mine. Yeah.
Simon: Oh yeah. I should, yeah. Should be yes, we should be accurate about that. Maryanne’s,
Maryanne: I’m using that word, but yeah, they are trying to normalize it, but they’re even saying, they’re trying to normalize it. This isn’t, if you know.
Don’t access it if you don’t want it, it’s there if you can. This is, everyone should be accepting this. And it, we get into freedom of conscience issues because of course, euthanasia is not isolated to that individual because it involves health practitioners. And if a person is living in a care home, it has implications for the care home for hospices, it has implication for hospices.
So this isn’t. You are an individual. If you wanna choose that, great. Go for it. It’s not gonna impact anyone else. This is quite different. It is. This is something that other people are impacted by.
Simon: It is certainly, one of the things I’ve often argued in the autonomy space, and you’ve just echoed it, is the person making the decision is never doing it alone, as you said, from the medical to the health practitioners, hospices, hospitals private, well, even some private facilities, but also the wider family.
There’s always a lot of other people impacting and coercion is one of the areas you touch on in your discussion paper as well. But let’s just tease some of that out, starting around. Conscience rights because one of the more disturbing elements for me coming out of the ministry’s review and what you address in your discussion paper, is the ministry wanting to remove conscience rights from individuals.
So thinking doctors and nurses, and they’re wanting to remove conscientious rights from the likes of hospices or entities. I mean, what is driving that you think from the ministry side?
Maryanne: This is not limited to the Ministry of Health here. This is an international issue. So conscientious objection is something that doctors are able to do legally.
So you, you cannot force someone to participate in something if there is a conscientious objection, right? And for both abortion and euthanasia, those are two things within the health system that there are those rights for. Other countries have these rights in Canada, and there’s been a court ruling that has actually overridden those rights.
So it’s not impossible to override them. The ministry doesn’t say it wants to override consu, just objection. But the way that it is framing its proposed changes is that if you are a doctor and you’ve got a patient who wants euthanasia, then you need to assist them in accessing it. So that means.
Providing you know, results, reports, stuff that, that would go into their paperwork and pointing them in the direction of someone who can perform it. Very few doctors perform euthanasia. There’s only a handful on the registered list, so it’s not like they know that not all doctors are going to participate in it.
Actively, but conscientious objection, rights. Acknowledge that by helping someone do something that you think is not in their best interest. It’s called moral injury. When you believe one thing, but you are compelled to do something else. And as a professional whose job is to care for people, that’s a really serious thing to put on someone.
So they’re not saying you have to be the one. Doing the injection, but they are saying we think that there shouldn’t be room for a doctor to step back and go, you know, there’s a national number you can call, you can get information there and then you know, wash their hands of it, which would allow a doctor to go, okay, I’m not aiding and abetting something that I actually think is not in this person’s best interest.
Simon: So why do you think they’re trying to fall? I mean, again, this is only a suggestion from the Ministry of Health. You, right. Again, touching on Canada is a very worrying example. I mean, we’ve held the right of conscience is one of our fundamental rights for a long time. Why do you think the ministry is so determined?
And that’s my word, but determined to, to remove conscience rights in this space? Knowing full well there will be that moral injury that you talk about.
Maryanne: Yeah, reading the report the wording that comes through it clearly paints a picture of their attitude is this is a consumer rights issue.
Healthcare is, we are consumers. Healthcare is something that is provided by the state. And words like patient, you know, and caregiver are absent. It is about a consumer, right? And so. In their framework, which is not a moral framework, it this is a government agency and they see if something is legal, then it is automatically good.
And if somebody wants something as a consumer, they should get it. Both of us heard Megan Vest the other week. She’s a palliative care expert and an ethicist from Australia. And so she’s been part of discussions there, as most states have legalized it. And one of the things that she highlighted, and it goes beyond euthanasia, but in, in the medical system at large, is this materialism, seeing our bodies like machines.
We’re just, you know. Bunch of components, and then you’ve got the doctors treating the broken machine and their machines themselves, they’re there to treat the patient and what the patient wants as a consumer is automatically good and right if it’s legal. And so you must do what they want. And it, it removes the complexity of going, actually we are integrated beings.
We’re mindbody and soul. And so we can’t look at it as simply as. Is it legal? Then a doctor should be fine with it and they can do it because we’re talking about ending someone’s life. This isn’t And it serious. I’m serious, doctor. Yeah. But because there’s no, no ethical kind of tearing of things. One option is as good as another is as good as another, and it just comes down to, you know, really obvious questions.
Like, like expense. Like what does the patient want? Now the added problem with that is there are not equal choices because not everybody has access to palliative care, which is the obvious good option for people who are suffering at their end of their life, who are terminal and who need pain relief and symptom control, and help walking through this.
This end of life stage because it’s not just about, oh, you’re gonna die and then you die there, there is an actual process and to die, well, it involves other people because we’re in a relationship with other people and those relationships are gonna end. It involves growing the way we do in every other stage of our life.
I mean, suffering is a part of life. And to say, well, we just need to take away the suffering, and then everything is fine. Well, you’re taking away the life as well. So there are questions around this. The ministry’s review doesn’t go and doesn’t touch on any of this complexity. It keeps it very simple and goes, if the patient wants it, they should get it.
The doctor’s there to provide a service.
Simon: It’s almost not a doctor then I would argue, I mean, I expect I better personalize it. Because you might have a different view and certainly others might is, you know, we want doctors to bring their whole self. So of course their medical knowledge, their training, their scientific understanding.
But we also want their empathy, their humanity, their ethics. And it worries me when we have. And we see this across a number of the medical ethical issues. Yeah. Doctors are just being reduced to functionaries, as you say, to machines. I think that should concern people because we expect more of our doctors.
And if these recommendations were to go ahead. I mean, from your research and your thinking, we’d probably see a number of doctors and nurses actually leave the profession that, that this would be a line they don’t want to cross.
Maryanne: Yeah. And this is something that the ministry should be addressing because even if it doesn’t want to weigh into ethical and moral matters, it needs to be aware of practical ones.
So when there’s one hospice in New Zealand that when euthanasia became legal, so yeah, will offer it here, only one. Hospice New Zealand Palliative Care Specialists, by and large do not think that euthanasia. Is necessary. The one that did, I had somebody who worked there tell me that they lost their lead nurse and a whole bunch of their staff, like over a dozen staff.
Medical staff left when they started offering euthanasia because those people didn’t want to work in an environment where people’s lives were being actively ended. They’re palliative care specialists now. This is one thing that, that Megan brought up. There has been a study done. This is back in 2016, journal of Contraception and Reproductive Healthcare.
The title of the journal article is, yes, we Can Successful Examples of Disallowing, conscientious Objection and Reproductive Healthcare. So this is dealing with abortion and they’re the way they address the problem of, well, some people who go into this field. Won’t want to participate is those people are able to find work in another field of medicine.
Not a problem, just they can work elsewhere if they’re not happy with it. But this is what it involves. Instead of recognizing that you are putting people under pressure, even if they don’t leave the field, there are a lot of people who don’t want to be participating in that. Conscientious rights have to be protected or you will lose people.
And already this event the other day. Just anecdotally, there are people talking about health. They have recognized that there are fewer people training for beginning of life stuff because they don’t want to be compromised. And there are people choosing not to you know, specialize in palliative care.
There are fewer and fewer palliative care specialists. And given the change in law there’s probably connection for some of them in that as well. They do not want to go into. A profession where lives are going to be actively ended, even if it’s somebody’s choice. Now, this is a field where we already have fewer than half as many palliative care specialists as we need in New Zealand.
We don’t want to be saying, well, they can just, they can work elsewhere. We don’t have enough to care for all of us. All are going to die. About 90% of us will be eligible for the kind of care that auspices offer. Do we want to drive people away from that profession? By saying we, we are going to mandate something that doesn’t need to be mandated.
Simon: I would argue that this shows it’s ideological the drive to actually force good doctors and nurses out of the profession in this case because they won’t practice euthanasia. And the same as actually in the abortion space is, yeah. The strongest signal that we’re dealing with an ideological drive here.
It’s not practical. It’s not feasible, it’s not economically sensible. But it’s ideological. There, there can be no resistance and it seems to me, Maryanne, the more radical the ethical issue is, the more the ideological drive to, again, force. People out. And I would make the argument, the Ministry of Health seems willing to accept that because their review, as far as I was reading, I didn’t pick up anything in there saying, oh, well if we remove conscience rights from doctors and nurses, they’ll leave.
Or some will leave in a system already under pressure.
Maryanne: Yeah. And you mentioned Care Homes they would like, and this is not currently legal at the moment, care Homes can choose whether or not they offer it on site. The ministry would like that to change again, to for ease of access so that if a care home doesn’t allow it onsite, they lose their registration.
I mean, that’s very heavy handed.
Simon: Oh, massively. So is a heavy handed, can you imagine
Maryanne: like taking hospices offline because. They won’t allow it on site. I mean, people can still access euthanasia, not in a care home. That might be their first choice. But there are lots of things that we want and don’t get because it’s not convenient to other people.
And so if people don’t want to live in a care home where people are being euthanized next door they shouldn’t have to. And it’s perfectly reasonable. In fact, the report said one of the options they considered is that. Care homes have to be upfront when people move in and say, look, we don’t provide euthanasia on site.
If you want to access that, you have to go elsewhere. And then let the person, the consumer, make the choice. And they disregarded that because it would limit access. So they said, we can’t do that.
Simon: I personally find it extraordinary, particularly in the autonomy. Argument or space in so far as if it’s an autonomous choice or rather one exercises their autonomy to choose euthanasia or assisted suicide.
Why is autonomy, if you will, or freedom not being given to the care homes, to hospices, to, to doctors their autonomy has been, or proposed to be aggressively removed? And I’m pleased you, you bring up the care homes. Yeah. If they. They could be shut down. I mean, that is an exceptionally yeah.
Aggressive move.
Maryanne: Yeah. And this is what, well, whoever’s writing it from the ministry I don’t, I don’t know what the balance of opinion is, but those who are behind the review, that’s their opinion. Yeah.
Simon: It’s just, again, the strong army and anti autonomy this is what I, well and anti
Maryanne: choice. One of the things I highlight here is not everybody has access to palliative care or hospices, which is by far the best option at end of life for anyone.
And there may be people, exceptions you can point to and go have an a, a legitimate argument about well would. Would euthanasia be more merciful because this person is suffering horribly and all the rest? And that’s another debate. But what you can’t debate is that palliative care is the best thing hands down for people at the end of their lives.
You don’t know. Suddenly it is keeping symptoms in check. It’s managing like these people are. Experts in managing pain. They counsel people as to, you know, the process, what to expect. So that eases people’s anxiety. They know what’s coming, and it brings the whole whanau in so people around them understand what’s going on.
Everybody is coached through something that’s quite foreign and scary to us. I mean, who, what else would you want? Not everybody has access to it. It’s not fully funded. So you’ve got people who, because euthanasia is fully funded, can access euthanasia and can’t access palliative care, that’s not great choice.
Simon: I think that’s something that needs to be and why. I really like your discussion payer. Because it drives that home. If you want to have a choice argument, and this is me. Paraphrasing if those who want to pursue the choice or the autonomy argument then palliative care needs to be an actual choice, which it isn’t for many.
I don’t have the numbers in front of me, but you know your paper better than I do. Seeing you wrote it, you had some percentages statistics around actually how many New Zealanders can access palliative care and it’s woefully low.
Maryanne: Yeah, and it’s really hard to get an exact number because it’s not like you definitely have it here.
You don’t here for children, Starship is the only place that offers paediatric palliative care. So if you’re outside of Auckland then that kind of care gets kind of patched together. And so if you find somebody who’s, oh, look at me, I think I’m doing thumbs down. If you find somebody sit hands.
Who is willing to offer?
Simon: No, I was just saying idea. I muted myself. It’s one of my big mis I was just saying it just brings a little bit of levity into what’s actually a a heavy topic.
Maryanne: I know. Otherwise we would not be smiling at all. Yeah, and the paediatric palliative care is a little bit. Tragic because that I mean, children do suffer from terminal illnesses and die.
And if you’re outside of the Auckland region, there’ve been some mainstream media has picked up some of these stories and it’s been really good. To highlight the fact that parents of kids outside of Auckland are really stuck if their kids are deteriorating because you have to find somebody who has the skills, who’s willing to treat them, and some people just can’t.
So it’s just patched together. Absolute numbers is really difficult to come up with. Roughly we have roughly half the number of specialists. Of those who died last year, about a third of those who would be eligible for hospice care accessed it. Some of those would’ve accessed specialized palliative care in a hospital.
Some might’ve accessed it some other way, but we’re rough. We roughly need twice as many easily as we currently have, and the number’s only going to increase, and we have. The line for palliative care specialists is going down and the line for demand is going up.
Simon: And as we have an aging population, I mean, obviously, you know, palliative care is not strictly linked to age, but obviously more people who are older people and approaching end of life need it. I mean, it’s almost scandalous. I would argue and I was talking to Tanya Kovich recently. She’s an MP who’s picked up a bill that myself and before that Maggie Barry had saying that we need to not only fund palliative care, but actually have a plan.
There isn’t even a palliative care plan around the country. And I think what really. Highlights. The problem in linking it even to the question of euthanasia is the review panel or review committee of the End of Life Choice Act. There are three people, as you know, they were noting access to palliative care in the rural areas was, well, it’s almost non-existent.
And that they had sort of a worrying concern, Maryanne, that. People were then seeking, more people in the rural areas were seeking euthanasia because they didn’t have access and the ministry blocked them from the necessary data to actually confirm or otherwise that suspicion. Yeah,
Maryanne: I didn’t know that bill was originally yours in Maggie’s before that.
I’m so pleased that Tanya has this bill in there and she’s made it better. I didn’t know what it before, but. It is just astounding that we can emphasize choice but not emphasize fully funding palliative care. So I’m really glad that bill’s in there. I hope it gets pulled and I hope there’s a discussion about it because there needs to be the level of commitment that the ministry has to making sure everybody connects as euthanasia should be the level of commitment there is to making sure everybody can access palliative care and it’s not there.
Simon: No. And we’re seeing from overseas jurisdictions that people end up, well euthanasia is seen as the easy, cheaper way out. Yeah, if you Yeah. Which is deeply worrying. And actually that leads me, your paper also talks about the recommendation, again, from the Ministry of Health to allow doctors to talk about euthanasia to patients.
At the moment, they’re not really allowed to seed the idea. I mean, talk us through why. You know, for some people going, well, why wouldn’t the doctor talk to me about this as an option in the same way they can give me pharmaceutical options? So what’s the issue here?
Maryanne: Yeah. And even though the legislation says they mustn’t, some do the reason the simplest way I can put it is if you’re going to a doctor for medical problem and you’re under stress already because you’re facing this challenge, and they say, have you considered euthanasia?
What is that going to do to your will to look into your treatment options? I mean, it just completely decimate the kind of hope that you need to face a challenge like that. And when it’s a doctor saying it, I mean, it’s bad enough when it’s somebody’s child or something, because then that puts the thought in somebody’s head, oh, if they think this is what’s best for me and they love me, then you know, if your doctor is saying it.
One of the stories that I I included in the paper comes from Dr. Katherine men’s. Book with the end in mind. She tells story after story af you know, she spent decades in palliative care and she shares individual stories and it illustrates how different personalities, different health problems and needs can be met in different ways.
One of the people she treated had been in the Netherlands young dad. The terminal, I think it was cancer and every ward round. Because he needed constant care for treatment manage to manage his symptoms. Every ward round somebody would bring up euthanasia with him. Because you know, the Netherlands, they’ve got very loose restrictions around it, and it’s been common for a while and it made him feel guilty.
He said he was dreading ward rounds because he knew that there would be this conversation again, and he knew that. By not taking it. He could be. Being a burden on his family. He felt like he was a coward for not taking it. Like there were all these, it wasn’t just a choice it was a burden for him. He literally ran away to the UK.
He had family in the UK. He went there with his wife and his daughter and spent two former peaceful months. In palliative care being cared for by Katherine Maddox, and when he did die, he slipped into a coma. His daughter was playing outside. It was peaceful. It was the kind of death that people would say they want.
It wasn’t with the stresses of the decisions and the pressure from the health system saying, well. Because at the end of the day, as soon as somebody raises euthanasia with you, having looked at your prognosis, and they say, have you considered this? There’s nothing else to read between the lines, but you may be better off debt.
Simon: Yeah. And a person in authority in this case. Yeah. And it’s one of the reasons why euthanasia advocates have always wanted doctors to do the terminations. I would suggest, because it gives the white coat of legitimacy. You know, I certainly raised it when I was on the select committee that, you know, it’s not actually, and I’m not going to go into the specifics, but actually it’s not that difficult.
The process that is used to kill someone, you don’t have to be a doctor, but of course, doctors give a legitimacy and they hold an enormous amount of. Power. Which I find is ironic for, again, those on the more progressive side of politics who push this. Because they’re always about power and hierarchy and you go, well actually having your doctor tell you that euthanasia is an option, legitimizes it seeds the idea.
And yeah, because it’s the doctor telling you, you go, well, maybe that is the right option. In the same way when the doc says to me, we’re going to give you these pills, I don’t question it usually. Okay, doc. Thanks very much.
Maryanne: Yeah. Yeah. And it, it is part of what we were talking about before. It’s not just putting an option on the table, it’s normalizing it.
If you wouldn’t mind me reading a section of the paper that I think I’m quoting some of the ministry’s review here and what it highlights is that it isn’t enough for it to be available. It needs to be accepted from their perspective. So I’m saying the Ministry of Health does not acknowledge that there are valid reasons to opt out of participating in euthanasia.
It identifies that quote, and this is from the review. Some communities, tikanga custom values are not aligned with or supportive of assisted dying and that some held the view that the UA spirit belongs to God and the body should be allowed to perish naturally. End quote. I say this belief shared not just by many Māori, but also by many faith communities, is one that the ministry considers misguided regarding mana, who consider euthanasia to be the same as suicide.
They write, quote, this is the ministry that this points to a lack of awareness and acceptability of assisted dying within our communities, and an urgent need for assisted dying to become familiar, understood, and accepted.
Simon: So we’re going to expect I’m being a bit facetious here but you know, are we going to expect to see struggle sessions from the Ministry of Health onto people that you all have to change your views.
You’ve got to come to understand that our take on euthanasia’s, right? I mean, that’s chilling. I have to say actually, Marianne.
Maryanne: Yeah, I mean, it’s legal, so it’s right. It’s as simple as that from their perspective. And so anybody who sees ethical or even practical problems with it will not have any sympathy from the ministry, which, if you’re a doctor working in that system is really hard.
Simon: Well, again it. I suppose my former political hat on, and even my philosophical one, it’s a deeply worrying dynamic because their view is, okay, there are differences of opinion. We’re not going to debate or discuss them. You are just going to have to change. You know, you’re just wrong. We are right. And we will use all the conversive power of the state including sacking you to make sure you understand.
I mean, it’s it, or understand the view as they, they have it. And again, all of this in the argument of autonomy and choice. Again I, yeah. Can never fathom Maryanne, how these guys cannot see the hypocrisy to be honest in their position, but it just deeply ideological.
Maryanne: Just and sorry.
I was just going to say, digging into that word choices, I mean, some of what I go into is just unpacking this idea of our choices being somehow sacred, when actually we change our minds all the time. So the fact that there isn’t a cool down period to consider this highlights the limitations on choice because actually good choice.
You, you take things into consideration when you’ve been given a terminal diagnosis and you’re in unchartered territory. You are not at your best when it comes to decision making. You would think that having a cool down period and. Have to see a psychiatrist, which now is only for people where there’s doubts about mental capacity and even then it’s just to make sure that somebody is competent to ascent.
It’s not to say, do you need some counselling? Do you need some help? This is a tough time you’re going through. That is not embedded in their framework for choice. It is entirely around expediting the process. The fastest time so far from application to death is two days.
Simon: Two days. Beause they make a big thing of it.
Sort of The average I think is 16 if memory serves me right. And feel free to, it depends. Two days
Maryanne: it depends. Yeah, like me mean median mode. There are some outliers at the upper end. So there published average is around three weeks, but actually the most common timeframe is two weeks. And yeah, two days.
I, I don’t see how that serves someone’s choices, you know, allowing it to happen that quickly, especially when, how can you check that there’s been no coercion and approve it and receive euthanasia in two days? I, the safeguards are on coercion. They’re there on paper. But when you look at what’s been going on and when you hear the testimony of two of the original three review committee members, you recognize.
That there are no safeguards against coercion. It’s what we don’t know can’t hurt us.
Simon: There are no safeguards at all. I actually, it’s been one of the things, one of my little drums I keep beating or ranting on my little soapboxes. There is no safeguards in the law. There’s a whole series of processes.
Yeah. Tick boxes. Yeah.
Maryanne: Yeah. Well, and when the tick boxes were blank the review committee members found that. There was information missing, and when they brought that to the ministry’s attention, the ministry said, I assume nothing’s wrong. If there’s no information. They’re the review committee if.
They are reviewing it, finding something missing, and then being told like with the higher numbers of rural applicants, and if they’re being told, oh, don’t worry about it. Well, what is a review committee for if they’re not to review it? They found that there was one person who’d been euthanized, who didn’t speak English, didn’t have an interpreter with them when they were having the consultation and was suspected of having dementia. How did that happen? And they didn’t get any answers.
Simon: No. And I think is one of the many reasons why effectively, I think one resigned from the review committee and the other who was raising questions did not have her time renewed. I. Because it was, yeah, inconvenience, and it wasn’t the word that I had in my mind when we started this chat, although I’ve used it a few times.
It’s ideology and I just can’t help feel we have ideological zealots. Again my opinion within the ministry pushing this because they believe it’s just normal healthcare. Just like going and getting, as I say, some neuro fend for your headache. This is just normal. Hence why they can’t tolerate.
Questions they can’t tolerate, actually people pushing back and why they want to snuff out the likes of conscience rights. This is deeply driven and it’s not medical or scientific, I would argue this approach. It’s not standing up to scrutiny.
Maryanne: No, because they would be taking, you know, the concerns of the review committee, for instance, seriously, they would be taking seriously the impact on staffing.
Like those are things that would be considered if this was balanced. But everything is driven by the fundamental need for quick and easy access throughout the whole review. That was the bottom line.
Simon: Which I’ve always found ironic. I mean, don’t get me wrong, we don’t, you know, in the broad sense, obviously I’m opposed to euthanasia conceptually, but it’s, you know, you don’t want people to be unnecessarily burdened.
But actually the current situation, I said it’s fully funded. There are few doctors, but enough of them, and I’ve always been struck Maryanne, that if you are a person deciding to end there. They’re alive and you’ve made all those, I don’t know, choices. You, you can, you know, travel just that little bit further if you need or wait just that little bit longer.
You know, this is an enormous decision and yet somehow the final steps have to be so easy, simple, and accessible, that ethical principles, things like conscience rights are just going to be tossed out the window.
Maryanne: Yeah.
Simon: Nutty, by the way. I’ve only just written about it in recent days, but the, this very same ministry of Health and I feel like I’m bagging the entire ministry.
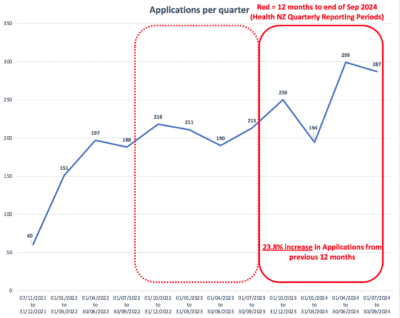
I, I shouldn’t be, but it’s really those who are behind this review. They can’t even count the numbers right. They’ve just updated some of their quarterly reports from last year and discovered in one quarter there were 56 more people who had died than they realized almost double the original.
Numbers. So, you know, the very ministry conducting this, again, I’ll use that word, ideological review can’t even tell us accurately how many people are being terminated. I mean, it’s just, it’s clearly ‘safeguards’ are not there or working.
Maryanne: Yeah. I saw that you guys were onto that and the sad thing is I wasn’t surprised and the.
We’re at a rate of not quite one a day. That should be pretty easy to keep track of, and this is somebody’s life ending, so it’s pretty consequential. I don’t know how they can’t keep just the basic count straight. Yeah. If they can’t do that, as you’ve pointed out, how are we trusting them to meet all these other requirements?
Simon: Well, you will know in the work to put this discussion paper together. The ministry says in its review that it’s all working perfectly. I don’t have it literally written verbatim in front of me, but in effect, they say that everything is fine working well. Yeah, and it’s like it’s demonstrably false.
We should end on a positive because of course, with all of your research and discussion. Papers In your work at Maxim, you have a variety of recommendations of how, you know New Zealand should move forward in this space. Do you want to quickly take us through those?
Maryanne: Yeah. I’ll get them in front of me so that I don’t miss any.
Simon: Yeah. It’s not a test, fortunately.
Maryanne: Yeah. So the bullet points are you’re,
Simon: as you’re pulling that together, actually, a side question, I mean, as someone who researches deeply into this space, how affecting do you find it? Obviously you’re a professional researcher, but you know, these are heavy topics. If you don’t mind me asking, how do you find it as you delve into these things?
Maryanne: I hadn’t dive deeply until kind of the end of last year. And I was pretty grumpy for a month or two. It was weird because I was reading and some of it, oh, I have book. If anybody wants an excellent book, Catherine Manix says, was the end in mind. I probably cried at Parts First Four chapter chapters and then some others.
Simon: It’s a great book. Highly recommend it.
Maryanne: Yeah, and it’s I’m making it sound like it’s sad, it’s enlightening. I feel like I understand the end of life and dying. Well, so much better. And there’s other good stuff out there as well. But she’s a genius. So reading that was a bright spot. It is just a little bit hard because you recognize that vulnerable people are made more vulnerable by the way this is being managed. And I was just, you know, reading a lot about death, which isn’t something we do all the time. But it’s good to be having these discussions and encouraging others to have these discussions.
Because I think it’s really important that we don’t just stay naive and stay ignorant because then we’re liable just to, to react emotionally. To the way things are phrased and worded and we become much more easy to manipulate instead of thinking deeply about these things.
Simon: Which is why I think the, again, the work you are leading, maxim’s leading and others in the space like Catherine’s book is so important.
And look, thanks for asking that because I know it’s a bit more. Personally, I know having for literally a couple of years when I was on the select committee and then the bill was going through Parliament at, you know, literally years of basically thinking about death and dying every day saying, oh God, I’m surprised I didn’t end up on any antidepressants or anything, but, you know.
Yeah. Tell us about your recommendations.
Maryanne: Yep. Well, the first is like we were talking about better information. I mean, our choices are dependent on the information we have and the actual options we are given. So the more we know about what a natural end of life entails, the stages our bodies go through and what options are available in the health system that’ll just improve things right away.
It’s called death literacy, providing universal access to palliative care is the second one. And I. Everybody, everybody would win if we could do that. And just encouraging people. It encouraged the system itself to be proactively training people in that area. Even other specialists can upskill in palliative care.
So that needs to happen through this prioritizing training, which I started going into. So we need the people to provide the palliative care. Hospice is obviously, yeah, just building that up and then fortifying the protections around euthanasia, and we have the most points around that because that’s really a pressing concern.
The ministry is clearly trying to remove some of those protections, and they’re not strong enough as they are.
Simon: No, it’s the irony of everything you’ve talked about all the evidence that’s actually coming forward in the public space. Anyone watching here can jump online and actually find, you know, not only of the discussion paper that Maryanne’s done, but all the problems that we’re identified and yet the pushing past those, ignoring those.
And to be fair too, it’s the politicians. So it’s not just, not just the ministry, but wanting to expand this. So it’s really good. You know, from my perspective, you talk about fortifying the position more is needed. So Maryanne, if someone wants to get hold of this paper and read it, and I highly recommend that people do.
Where do they go?
Maryanne: They go to maxim.org.nz and there’s a little tab with our research. You can also go onto the website and just sign up to receive our monthly bulletins. And anytime we put out something like this, you’ll get it
Simon: and I’d highly encourage our viewers to do so because the work that Maryanne and the team there at Maxim do is.
Fantastic. And wide ranging. But look, Marianne, very grateful for your work and research and again, you know, these are heavy topics. So grateful for you taking that time just to yeah, chat with me about them and being part of the show.
Maryanne: Thankful for you, Simon. I really appreciate it.