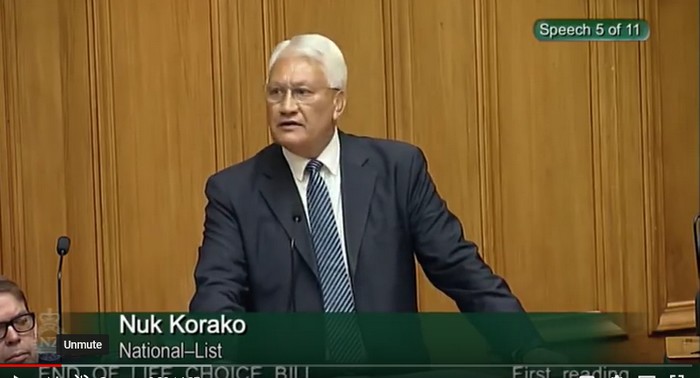
I believe this is a sad day for the House. We are here talking about the State sanctioning killing of New Zealanders. This bill suggests that suicide is a solution under certain circumstances, and I stand today to reject this.
I spent two and a bit years chairing the Health Committee as over 21,000 Kiwis from across the spectrum spoke to us, and 80 percent, who had well considered it, said no. I’ve studied philosophy and human rights, I’ve been at hospital beds and hospices, I’ve seen more death and suffering than sometimes I care to remember, and, fundamentally, I do not believe doctors should be killing their patients.
Members of the House, this bill is about killing in two ways. The first is called euthanasia. It’s where the doctor takes an injection, usually something like phenobarbital, and injects it into you—only after they’ve sedated you, of course; couldn’t have the inconvenience of twitching. The other is physician-assisted suicide, where, again, they give you a massive dose of drugs. You take that yourself, at your own choosing—and hope that the kids don’t find it in the medical cabinet at the time.
This bill combines both of those. That’s almost unheard of in any other jurisdiction around the world. This bill before us tonight is the worst example of euthanasia legislation in the world. I say that as someone who has looked at every piece of legislation.
Where it starts, really badly, is clause 4. We hear it a lot: it’s all about terminal illness, up to six months. But the doctors, the medical people, will tell you that six months is just an indication; it’s not a guarantee. And the doctors will tell you too that they misdiagnose all the time.
They also talk in this bill about irremediable, grievous conditions. That’s incredibly broad, undefined. What is “irremediable”? What is “grievous”? Basically, it includes everyone, including those with disabilities.
But the bill also, rather insidiously, talks about suffering that a person deems intolerable—what you deem intolerable. Sorry, Mr Speaker—what members may deem intolerable. This is a clear indication that it is the courts who will be making decisions and choices, not this Parliament and certainly not the person.
In the debate in this space, I’ve often said, it’s between choice and public safety. Let’s be very clear: the current laws as they stand mean that no one will die against their will, but this proposed law that we consider tonight will make involuntary deaths possible. We know in this House we do not make things perfect, because changing this law will allow some to assist the suicide—well, sorry. People who choose to assist in suicide will put others at risk.
We know that this law applies to everyone. It does not apply simply to the rational and articulate; it applies to the elderly, the disabled, the sick, the vulnerable—all of us. Not everyone is fortunate enough to live with a loving, caring family. Not everyone has a doctor fully in tune with them and their needs. This law will apply to the depressed, the lonely, those who feel a burden, the disabled, the fearful. I should point out that these are the same feelings of a 16-year-old who is keen to suicide, the 40-year-old who has lost their farm, or the 80-year-old on the deathbed.
I repeat again, as I did a few months back, that you cannot stand in this House and decry the suicide of one group of people—say, the youth—and then encourage the suicide of another group—say, the sick. They are the same feelings that are there. And I don’t say it alone. It’s very easy for the media and others to attack, but, actually, this is the opinion of the major medical groups, the psychologists, and the youth workers. I add their voice tonight.
There’s a lot of talk about choice. Let me say one thing about choice: the patient in this space never makes the choice. If they did, there wouldn’t need to be doctors and psychologists and boards and panels. The doctors make the choices. The family makes the choices.
If you think I’m exaggerating, go and look up an example in the Netherlands recently. A woman with dementia who, yes, years ago, had said that she would like to die by assisted suicide, was held down after being sedated by her doctor and family—they put drugs in her tea. They sedated her, held her down as she screamed and yelled, and then they killed her. The doctor was able to report it, and they just said, “Oh, well, you acted in good faith, but she’s dead now.” So much for the choice and autonomy that she exercised.
And I’d point out too that if it’s about choice and autonomy, we all have it. If it’s a human right, all humans have it. There is a slippery slope, and one only needs to turn to Canada, which has already been mentioned, which is already pushing the boundaries.
There are no safeguards; there are just lots of criteria. Being 18 is not a safeguard. All the reporting comes after the fact. If you get it wrong, the person’s still dead.
Doctors don’t want to be part of this. The few that do will make a business of it, and there will be doctor-shopping. The conscience rights in this bill are a nonsense. If you oppose, the doctor must hand that person over to someone who will.
It’s a very, very poor bill, and, fundamentally—thousands of health professionals and others have argued in the recent public debate—this is an issue where the public safety will be put at risk. So I ask this House how many involuntary deaths and errors are we willing to accept through this law: one, five, 10—