MD Magazine 7 July 2018
Family First Comment: An excellent summary…
#protect
www.rejectassistedsuicide.nz
Introduction
In an age of “alternative facts,” it’s hard to sort out myth from reality when it comes to so-called “medical aid in dying” (MAID), also called physician-assisted suicide (PAS). By whatever label we attach to it, this practice involves a physician’s prescribing a lethal drug for a patient with a putatively terminal illness who is requesting this “service.” Some form of MAID/PAS is now legal in 5 states and the District of Columbia.
People of good conscience, including many physicians, are sharply divided on the ethics of MAID/PAS. Unfortunately, much of the support for this practice is founded on several myths and misconceptions regarding existing MAID laws and practices. Here are 12 of the most common.
1. Everyone has a “right to die,” including a right to take one’s own life, acting alone or with assistance.
In contrast to “liberties,” rights entail the cooperation or assistance of others.1 Mentally competent people may be at liberty to end their own lives (ie, will not be prosecuted), but there is no recognized right to suicide that involves the cooperation of others. In Washington v Glucksberg (521 US 702 [1997]), the US Supreme Court (USSC) denied that there is a constitutionally protected “right to commit suicide” or a right to PAS. To rule otherwise, the majority held, would force them to “reverse centuries of legal doctrine and practice, and strike down the considered policy choice of almost every state.”
That said, the USSC has held that all competent persons have the right to refuse unwanted or “heroic” measures that merely prolong the dying process.2 Similarly, in Vacco v Quill (521 US 793 [1997]), the USSC held that there is a legal difference between withdrawal of care and provision of a lethal intervention; ie, everyone has a right to refuse medical care, but no one has a “right” to receive a lethal means of ending one’s life.
2. People who request MAID usually do so because they are experiencing severe, intractable pain and suffering.
Most requests for MAID are not made by patients experiencing “untreatable pain or suffering,” as data from Oregon have shown; rather, the most common reasons for requesting medical aid in dying were loss of autonomy (97.2%), inability to engage in enjoyable activities (88.9%), and loss of dignity (75.0%).3
Many patients who request assisted suicide are clinically depressed and could be successfully treated, once properly diagnosed.
3. In states such as Oregon and Washington, where PAS is legal, there are adequate safeguards in place to ensure proper application of the PAS law.
In Oregon, reporting to the state is done solely by the physician prescribing the lethal drugs, who has a vested interest in minimizing problems. Moreover, if a physician was negligent in making the initial diagnosis or prognosis, there is no way to track this, since, by law, all death certificates will state that the person died of the putative underlying disease. At the same time, the physician is rarely present at the time the patient ingests the lethal drug, so the possibility of abuse—eg, by coercive family members—cannot be adequately assessed.
The Oregon department of human services has said it has no authority to investigate individual death-with-dignity cases,4 and Oregon has acknowledged that its law does not adequately protect all people with mental illness from receiving lethal prescriptions.5 Thus, it is nearly impossible to determine cases in which, for example, terminally ill patients were pressured to end their lives by family members. A study in Michigan Law Review (2008) found that “seemingly reasonable safeguards for the care and protection of terminally ill patients written into the Oregon law are being circumvented…[and that]…the Oregon Public Health Division (OPHD), which is charged with monitoring the law…does not collect the information it would need to effectively monitor the law…OPHD…acts as the defender of the law rather than as the protector of the welfare of terminally ill patients.”6
Kenneth R. Stevens Jr, MD, and William I. Toffler, MD, both of the Oregon Health & Science University, point to other actual or potential abuses in PAS-permissive states, including “physician shopping” to get around safeguards; nurse-assisted suicide without orders from a physician; and economic pressures to use PAS, such as Oregon Medicaid patients being denied cancer treatment but offered coverage for assisted suicide.7Furthermore, an investigative piece by the Des Moines Register revealed that mandatory reporting requirements were not followed by hundreds of doctors in states where MAID/PAS is legal.8
4. In the United States, only people with terminal or incurable illnesses are eligible for PAS.
Most PAS legislation applies to an adult with a terminal illness or condition predicted to have less than 6 months to live. In Oregon and Washington State, nearly identical criteria are interpreted to mean less than 6 months to live—specifically, without treatment. Thus, a healthy 20-year-old with insulin-dependent diabetes could be deemed “terminal” for the purpose of Oregon’s Death With Dignity Act.
So, too, patients refusing appropriate treatment may be deemed “terminal” under current interpretation of the Oregon law. Thus, a patient with anorexia nervosa who refused treatment could be eligible for PAS under Oregon law, even though she could recover with intensive therapy. As Swedish investigator Fabian Stahle observes, “This is in fact an alteration of the traditional meaning of the concept of ‘incurable.’”9
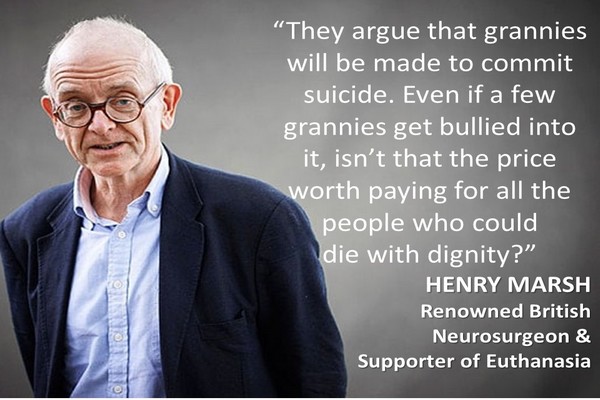
5. Slippery slope arguments against PAS are overblown. In European countries that allow PAS, there is no evidence that patients are being euthanized improperly.
People with nonterminal illnesses have been legally euthanized at their own request in several countries for nearly 15 years. This has included certain eligible patients who have only psychiatric disorders. In 2002, Belgium, the Netherlands, and Luxembourg removed any distinctions between terminal and nonterminal conditions—and between physical suffering and mental suffering—for legally permitted PAS. Between 2008 and 2014, more than 200 psychiatric patients were euthanized by their own request in the Netherlands (1% of all euthanasia in that country). Among them, 52% had a diagnosis of personality disorder, 56% refused 1 or more offered treatments, and 20% had never even had an inpatient stay (1 indication of previous treatment intensity). When asked the primary reason for seeking PAS/euthanasia, 66% cited “social isolation and loneliness.”
Despite the legal requirement for agreement between outside consultants, for 24% of psychiatric patients euthanized, at least 1 outside consultant disagreed.10-12
The United States has not been immune to the slippery slope, either. For example, in Oregon, a psychiatrist opened a fee-for-service death clinic where, for $5,000, “terminally ill patients who are eligible to take advantage of…Oregon’s suicide law can book a death that might look a lot like a wedding package.”13
6. The method of “assisted dying” now used in Oregon and other PAS-states assures the patient of a quick, peaceful death, without serious complications.
A peaceful death is by no means guaranteed using current methods of PAS, as a recent piece by Lo pointed out14: “Physicians who support PAD need to consider how to address the potential for adverse outcomes, including longer time to death than expected (up to 24 hours or more), awakening from unconsciousness, nausea, vomiting, and gasping.”
Data collected between 1998 and 2015 showed that the time between ingestion of lethal drugs and death ranged from 1 minute to more than 4 days. During this same period (1998-2015), 27 cases (out of 994) involved difficulty ingesting or regurgitating the drugs, and there were 6 known instances in which patients regained consciousness after ingesting the drugs. However, it is difficult to know the actual rate of drug-induced complications, because in the majority (54%) of cases between 1998 and 2015, no health care professional was present to attend and observe the patient’s death.15
7. “Death with dignity” comes down to the patient’s autonomy and the right of patients to end life on their terms.
In the first place, under current legislation permitting so-called medical aid in dying, the patient is completely dependent on the judgment, authorization, and prescriptive power of the physician—hardly a state of autonomy.1 Moreover, autonomy is just 1 of the 4 “cornerstones” of medical ethics; the others are beneficence, nonmalfeasance, and justice. As Desai and Grossberg observe in their textbook on long-term care:
“The preeminence of autonomy as an ethical principle in the United States can sometimes lead health care providers to disregard other moral considerations and common sense when making clinical decisions…we strongly feel that the role of the medical profession is to understand but not to support such wishes [for physician-assisted death]. Every person’s life is valuable, irrespective of one’s physical and mental state, even when that person has ceased to deem life valuable.”16
8. Doctors who conscientiously oppose PAS are perfectly free to refuse participation in it.
In theory, the California guidelines state, “[a] healthcare provider who refuses to participate in activities under the act on the basis of conscience, morality or ethics cannot be subject to censure, discipline…or other penalty by a healthcare provider, professional association or organization.”17 However, prior to its PAS law being declared unconstitutional, physicians in California could be compelled to participate in PAS under certain circumstances.
California’s health department regulation requires a state facility to provide PAS. If the request is denied, the patient has a right to a judicial hearing on the matter. If the court determines the patient is qualified, the attending physician must write a prescription for lethal drugs.18 Moreover, there is evidence that physicians are sometimes pressured or intimidated by patients to assist in suicide.7
9. Terminally ill people who request MAID are not suicidal and don’t commit suicide. They are dying and simply want “hastening” of an inevitable death. In contrast, genuinely suicidal people are not dying of a terminal condition, yet they want to die.
This argument plays fast and loose with language, logic, and law. In fact, it turns ordinary language on its head, thereby eliminating suicide by linguistic fiat. As the American Nursing Association states, “suicide is the act of taking one’s own life,”19 regardless of the act’s context. There may indeed be different psychological profiles that distinguish suicide in the context of terminal illness from suicide in other contexts, but that does not overturn the ordinary language meaning of suicide. Thus, when a terminally ill patient (or any other person) knowingly and intentionally ingests a lethal drug, that act is, incontrovertibly, suicide.
Most suicides occur in the context of serious psychiatric illness. Yet patients who express suicidal ideation in the context of a condition such as major depression rarely want to die; rather, as numerous suicide prevention websites note: “Most suicidal people do not want to die. They are experiencing severe emotional pain, and are desperate for the pain to go away.”20
10. People requesting PAS are carefully screened by mental health professionals to rule out depression.
Most PAS statutes modeled after the Oregon Death with Dignity statute do not require examination by a mental health professional, except when the participating physician is concerned and decides to do so. Specifically, “[t]he patient is referred to a psychologist or psychiatrist if concern exists that the patient has a psychiatric disorder including depression that may impair judgment.”21
A study of the Oregon law concluded that “[a]lthough most terminally ill Oregonians who receive aid in dying do not have depressive disorders, the current practice of the Death With Dignity Act may fail to protect some patients whose choices are influenced by depression from receiving a prescription for a lethal drug.”21
In Oregon, 204 patients were prescribed lethal drugs in 2016 under the Death with Dignity statute, yet just 5 patients were referred for psychiatric or psychological evaluation.22
11. Doctors who participate in PAS are almost always comfortable doing so and rarely regret their decision.
Many doctors who have participated in euthanasia and/or PAS are adversely affected—emotionally and psychologically—by their experiences. In a structured, in-depth telephone interview survey of 38 US oncologists who reported participating in euthanasia or PAS, nearly a quarter of the physicians regretted their actions. Another 16% reported that the emotional burden of performing euthanasia or PAS adversely affected their medical practice.23 For example, 1 physician felt so “burned out” that he moved from the city in which he was practicing to a small town. Similarly, reactions among European doctors suggest that PAS and euthanasia often provoke strong negative feelings.24
12. For terminally ill patients, the only means of achieving death with dignity is by taking a lethal drug prescribed by one’s doctor.
Just a small minority of persons with a terminal disease seek a physician’s prescription for a lethal drug. It is not clear why self-poisoning confers more dignity to one’s death than more traditional and much more common ways of dying. Many people who are dying choose to “bear with” their pain. Some seek hospice care and—in cases of severe, intractable pain—merit palliative sedation.25
Some choose voluntary stopping of eating and drinking (VSED), which, according to a study involving hospice nurses, results in a more satisfactory death than seen with PAS. In fact, “as compared with patients who died by PAS, those who stopped eating and drinking were rated by hospice nurses as suffering less and being more at peace in the last 2 weeks of life.”26
A form of VSED called “sallekhana” has been practiced in Jainism for centuries and is regarded as an ethical and dignified means of achieving a “natural” death.27
Conclusion
The case for PAS legislation rests on a number of misconceptions, as regards the adequacy, safety, and application of existing PAS statutes. The best available evidence suggests that current practices under PAS statutes are not adequately monitored and do not adequately protect vulnerable populations, such as patients with clinical depression. The American College of Physicians,28 the American Medical Association, the World Medical Association, and the American Nurses Association have all registered opposition to PAS.
It is critical that physicians inform themselves regarding the actual nature and function—or dysfunction—of medical aid in dying legislation. The first step is to recognize and challenge the many myths that surround these well-intended but misguided laws.
https://www.mdmag.com/medical-news/twelve-myths-concerning-medical-aid-in-dying-or-physicianassisted-suicide